By Nancy Alexander, PT, CSCS
It’s complicated. It really is. The shoulder area (or shoulder complex as it is rightly called) consists of four bones; four joints; multiple ligaments; multiple muscles, and a bursa sac. It is unique and complex which leads it to be one of the most injured parts of our body. Today we will learn more about its structure and identify some of the most common conditions causing your pain and injuries to this area. We will also identify key activities for your recovery.
Structure
Bones of the shoulder include the breast bone (sternum), collar bone (clavicle), shoulder blade (scapula) and the arm bone called the humerus. The shoulder girdle (or complex) consists of the following joints: sternoclavicular (SC), acromioclavicular (AC), scapulothoracic joints, and the glenohumeral. Please see the picture below for a global view of the shoulder.
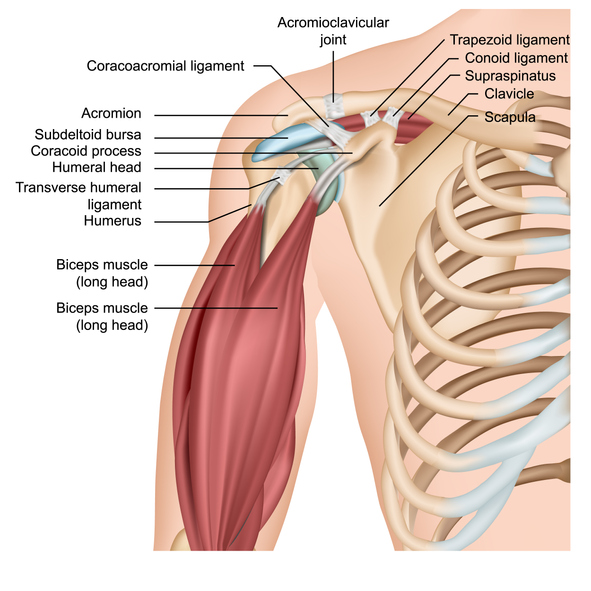
The glenohumeral joint is what most people think of as the shoulder joint. And rightfully so as it is the major joint of the shoulder and the focus of this article. This joint is where the top (or head) of the humerus meets up with the socket made by the scapula (the socket is called the glenoid fossa). It is built for mobility as it has a very shallow structure. This construction allows for circular movement of the arm.
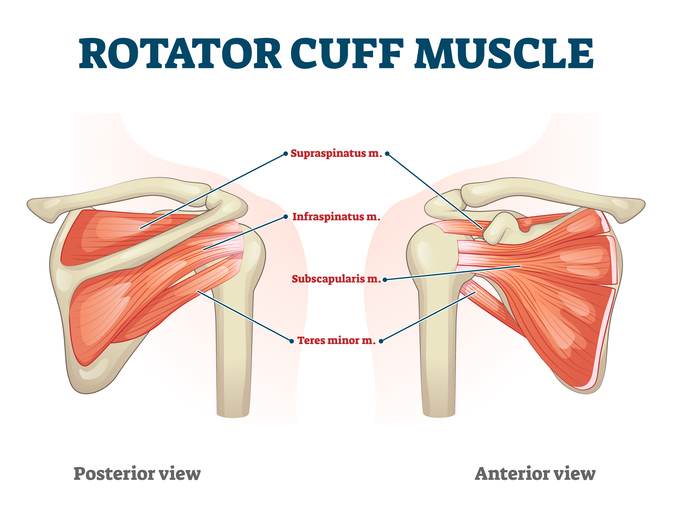
If this is so shallow, you might wonder what keeps it intact and strong. It’s all about the rotator cuff – a group of four muscles/tendons that attach to the head of the humerus. It may help to know that a muscle becomes a tendon as it approaches and inserts into a bone. Therefore, the name of the muscle and its tendon are the same. The four muscles/tendons are supraspinatus, infraspinatus, subscapularis and teres minor.
Not only does this group of muscles give stability to your joint, but they have added responsibilities for certain movements of your arm. The rotator cuff is in charge at this joint as these muscles support and stabilize the most flexible joint in your body. It is responsible for a wide range of movements from brushing your hair to pitching a ball. The extensive use of these muscles makes them more prone to injury.
Injuries may be mild or serious. How do you know when you need help fast with a shoulder injury? Here are symptoms that can indicate a more serious injury:
- Sudden and sharp pain.
- Decreased range of motion (that is, you are unable to move your arm away from your side).
- Pain along with swelling or bruising.
- Pain that consistently prevents you from falling asleep or wakes you up.
- No pain relief after several days of rest, icing and over-the-counter anti-inflammatory medications.
Common Conditions
Not all injuries or symptoms are serious. Some are successfully treated conservatively and these are included below. Be sure, though, that the most common cause of shoulder pain occurs at the rotator cuff. Often, this is when rotator cuff tendons become trapped under the bony area of the shoulder called the acromion. This space is critical to good shoulder health. It is small and thus you need to preserve this space as best you can. When the rotator cuff tendons become irritated, inflamed or damaged, rotator cuff tendinitis or bursitis can result.
There are other conditions, too. But please know that shoulder paincan have causes that aren’t due to underlying disease. Examples include overuse, disuse, sprain, strain, or even sleeping on your side.
Here are the eight most common conditions that cause shoulder pain:
1. Rotator cuff tear
This is a tear – either partial or full thickness – of one or more of the rotator cuff tendons that connects to your arm bone. (Recall that a tendon is what connects a muscle to bone.)
A tear can happen in a single event like a fall. Or it may slowly deteriorate over time due to repeated motion, bones spurs or other degenerative conditions.
Night pain is a classic symptom of a rotator cuff tear and often you will not be able to sleep on the affected side. Pain may be on the outside of your arm, down below your shoulder even though the tear is higher and at the shoulder. This is called referred pain and is common.
Initial treatment can include rest, ice, anti-inflammatory medications and physical therapy. Surgery may be required for a significant tear.
2. Rotator cuff tendonitis
This is when one or more of your rotator cuff tendons becomes inflamed. Often overhead activities can be the cause.
Treatment can include rest, ice, and anti-inflammatory medications. Most recover within a few weeks. Some may benefit from physical therapy.
3. Bursitis
There exists small fluid filled sacs strategically placed throughout our body and this includes the shoulder. Located directly under the acromion, this bursa acts as a cushion to reduce friction and facilitate normal and smooth motion. Overuse of your shoulder or keeping it in an awkward position over a period of time can aggravate the bursa, leading to pain and inflammation.
Bursitis often occurs right along with tendonitis and presents with similar pain as noted above. The treatment plan is the same as well and may also include injections of pain and anti-inflammatory medications.
4. Shoulder impingement syndrome
If one of more of the above conditions occur, it may lead to what is called shoulder impingement. Swelling can lead to “pinching” of your tendons in an already tight space.
This can cause considerable pain and will be worse in more provocative positions when pressure on these structures is increased.
Symptoms may last a few weeks to a few months. Treatment can include rest, ice, anti-inflammatory medications and physical therapy.
5. Frozen shoulder
Also referred to as adhesive capsulitis, this results in multi-directional movement restrictions as muscles, tendons, and ligaments inside the shoulder become thick and stiff. This makes most any movement painful and difficult.
Some develop this condition after an injury, but often many can’t recall an injury. It is seen more frequently with patients who have diabetes and some other conditions for reasons that aren’t clear.
Frozen shoulder may take months to resolve, even with aggressive treatment. Exercises and stretches can be useful to keep your symptoms more under control.
Please note, the onset of stiffness in your shoulder following a period of immobilization (such as with use of a sling after a fracture) is a different condition than frozen shoulder. Post-injury stiffness typically responds fairly quickly to physical therapy.
6. Calcific tendonitis
This develops when calcium deposits build up on tendons in your shoulder. The bigger they grow, the more painful they get.
These deposits can be seen on x-rays and can be the result of chronic rotator cuff tendonitis. Treatment usually includes physical therapy, non-steroidal anti-inflammatory medications and steroid injections.
7. Shoulder osteoarthritis (OA)
Similar to OA in other parts of the body, pain is produced by a deterioration of cartilage that covers the ends of your bones. This is often described as a deep ache that develops slowly over time. Most report no specific cause.
Treatment can be similar to a rotator cuff tear. But if severe enough, you can undergo a shoulder joint replacement which is similar to a joint replacement of the hip and knee.
8. Bone spurs
These can occur elsewhere in the body besides the shoulder and are often associated with OA. Also called osteophytes, they are a bony projection where once was a smooth bony surface.
A bone spur in the shoulder is often problematic and painful dependent on its position. If it is located on the underside of the acromion, this tends to further narrow the space above the glenohumeral joint. As a result, the spur can rub on rotator cuff tendons causing them to be damaged and even frayed over time.
Early on, posture correction and activity modification can help. Treatment usually includes physical therapy, non-steroidal anti-inflammatory medications and steroid injections. Ultimately surgery may be considered if conservative measures fail.
Recovery
Treatment for shoulder pain and injury, as with anything else, varies based on severity. Conservative treatment is often the first course of treatment such as anti-inflammatory medications, activity modification and ice as noted above. Not only will this help you feel better but inflammation takes up space. And space in your shoulder is at a premium. Anything you can to do free up needed room will help accelerate your recovery.
Activity modification includes reducing or eliminating aggravating activities or movements to help reduce symptoms early on in your recovery. As hard as it may seem to be, it is also very important to limit laying on the side of the affected shoulder. Laying on your side decreases the space under the acromion by at least half. This is huge! Even if you can’t eliminate it completely, decreasing your time spent here is time well spent.
If you choose to sleep on the opposite side, prop your top arm with pillows (folded pillows if needed) to be sure that arm is close in height to the top shoulder. This will also maximize space on the affected side.
Here are some other ways to enhance your recovery:
Posture
Do your best to sit up or stand up tall while keeping natural curves at your back as this will help maximize space at your shoulder. Try to avoid shoulders rounded forward as this is also a great strategy for the same reason.
Stretching
Stretching key muscles will help you restore range of motion, normalize joint forces, and make you feel better. Whether it is pain or inactivity, both can play a role in tightening (or shortening) structures over time.
Strengthening
Strengthening affected muscles will help you restore function and return to normal activities of daily living. This can be done two ways:
Scapular stabilization – strengthen the muscles that attach at your shoulder blade. The stronger your upper back is, the more efficient and effective your rotator cuff will be.
Rotator cuff strengthening – Target strengthening to your rotator cuff muscles to restore proper movement that leads to optimal future joint health and function.
Shoulder pain is common and can affect anyone of all ages. There are many more reasons for shoulder pain that are not included here. These simply are the most common. Seek consult from your physician and/or your movement specialist if you suspect injury here so you can get treated right away. Early treatment can help you avoid more serious injury later. Pay attention to your posture and include stretching and strengthening to your exercise program to help prevent overuse and strain to this area.

Leave a Reply